Pudendal Neuralgia : Causes, Symptoms and Treatment
Living with chronic pain can be debilitating, especially when it affects sensitive areas of the body. This is the case with pudendal neuralgia, a distressing condition causing pelvic and genital pain. While the condition is rare, its effects can severely diminish one's quality of life.
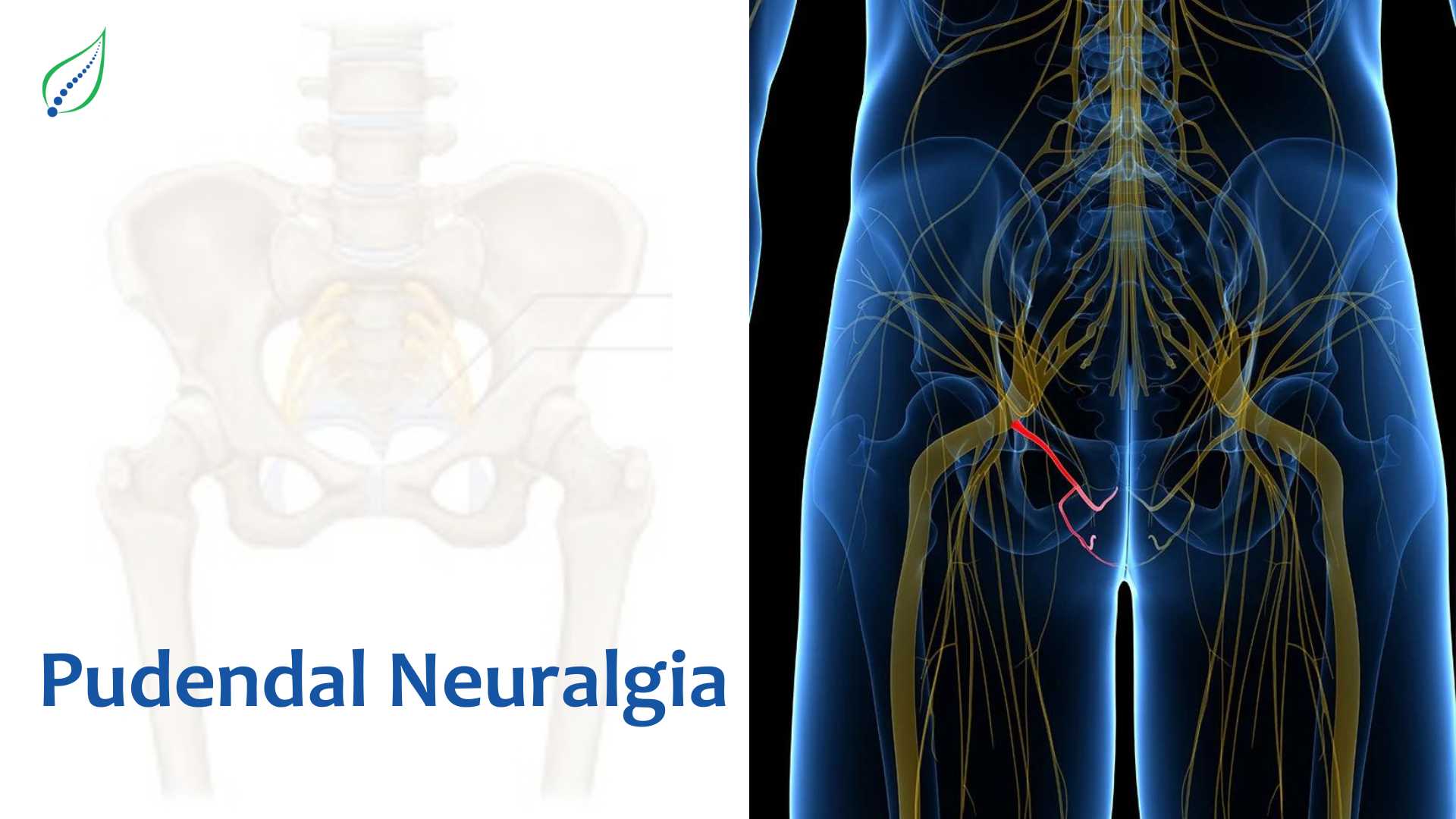
What is Pudendal Neuralgia?
Pudendal neuralgia arises from irritation or damage to the pudendal nerve, a major nerve running through the pelvis and providing sensation to the genitals, anus, rectum and nearby regions. When this nerve becomes compressed or inflamed, it results in the intense neuropathic pain that characterizes pudendal neuralgia. From sitting to using the bathroom, daily activities become agonizing.
While there is currently no cure, various treatments can provide relief and hope. In this blog, we will shed light on this often-misunderstood condition by exploring its symptoms, causes, diagnosis and current therapies. By raising awareness and understanding of pudendal neuralgia, we aim to help those impacted live fuller, more active lives. Armed with knowledge, patients can better advocate for their health.
Let's dive in and illuminate this painful disorder starting with how it manifests.
Symptoms
Pudendal neuralgia causes pain in the pelvic region supplied by the pudendal nerve. This nerve provides sensation to delicate areas like the genitals, perineum, rectum and anus. When it becomes damaged, it results in the following symptoms
- The primary symptom is pelvic pain affecting the pudendal nerve sensory zones. This can include pain in the:
- Genitals (vulva, labia, clitoris, vagina, penis, scrotum)
- Perineum (area between genitals and anus)
- Rectum
- Anus
- The pelvic pain may feel like:
- Burning
- Stabbing, shooting
- Crushing
- Prickling, pins and needles
- The onset of pain may be gradual or sudden.
- Pain may be constant or intermittent.
- Typically, worse when sitting, improves when standing or lying down since sitting puts pressure on the pelvis.
- Other possible symptoms:
- Numbness in the pelvic area
- Increased sensitivity - clothes rubbing on area is painful
- The feeling of swelling or a lump in the perineum.
- Frequent urination or urgency.
- Pain during sexual activity.
- Orgasm difficulties.
- Erectile dysfunction in men.
- Seeking medical advice promptly at the onset of symptoms is important, as the condition may worsen if left untreated. Early treatment is most effective.
Causes
There are several possible causes of pudendal neuralgia, including:
- Entrapment or compression of the pudendal nerve by nearby muscles, ligaments or scar tissue. The pudendal nerve can become trapped or compressed by anatomical structures surrounding it in the pelvis, like muscles, tendons or scar tissue from prior injury or surgery. This puts pressure on the nerve.
- Repeated minor damage from extensive sitting, cycling, horseback riding, or chronic constipation. Frequent repetitive actions like prolonged sitting, extensive cycling, horseback riding or chronic straining from constipation can cause minor injury to the pelvic area. This accumulates over time and damages the pudendal nerve.
- Previous pelvic surgery may have impacted the pudendal nerve. Past surgical procedures done in the pelvis, like for urinary incontinence or colon issues, could have directly injured the pudendal nerve located in that region.
- Fractures of the pelvic bones from major physical trauma can potentially damage nerves running through the pelvis, such as the pudendal nerve.
- During vaginal delivery, the pudendal nerve can become overstretched or compressed, leading to postpartum pudendal neuralgia.
- Noncancerous or cancerous growths pressing on the nerve. Benign tumours or cancers growing in the pelvic region may end up compressing the pudendal nerve if they become large enough.
- In some cases, no definite cause can be identified. For unclear reasons, some individuals develop pudendal neuralgia without any identifiable source of nerve injury.
These are the most common causes of pudendal neuralgia. However, your doctor may also find more than one or a new cause for this condition.
Treatment Options for Pudendal Neuralgia
Treatments for pudendal neuralgia aim to alter pain signals and reduce inflammation or compression of the pudendal nerve. Options may include:
- Avoiding activities that aggravate pain, like cycling, sitting too long, or straining during bowel movements. Refraining from actions that exacerbate symptoms, like extensive bike riding, prolonged sitting, or pushing hard during bowel movements, can help calm inflammation.
- Nerve pain medications instead of ordinary pain relievers which specifically targets neuropathic nerve pain work better than general over-the-counter painkillers.
- Physiotherapy exercises to relax pelvic floor muscles. A physiotherapist can provide exercises that stretch and relax the pelvic floor muscles and other muscles that may be compressing the pudendal nerve.
- Steroid injections to reduce inflammation around the nerve. Injections delivering steroid medication around the pudendal nerve may help relieve inflammation and swelling affecting the nerve.
- Pain management programs for coping techniques and tailored treatment. A multidisciplinary pain program can help patients manage symptoms through techniques like biofeedback, counselling, and customized treatment plans.
Conclusion: Pudendal neuralgia is a distressing condition causing chronic pelvic and genital pain when the pudendal nerve is damaged or inflamed. Diagnosis involves testing to pinpoint nerve issues. Treatments like nerve pain medication, injections, and physiotherapy can provide relief. While pudendal neuralgia can be challenging to manage, a combination of lifestyle changes, pain therapies, and expert guidance can help sufferers regain their quality of life. Speaking with a doctor at the first signs of pain is key, as early treatment leads to better outcomes.
_1749797551_1751826891.png)