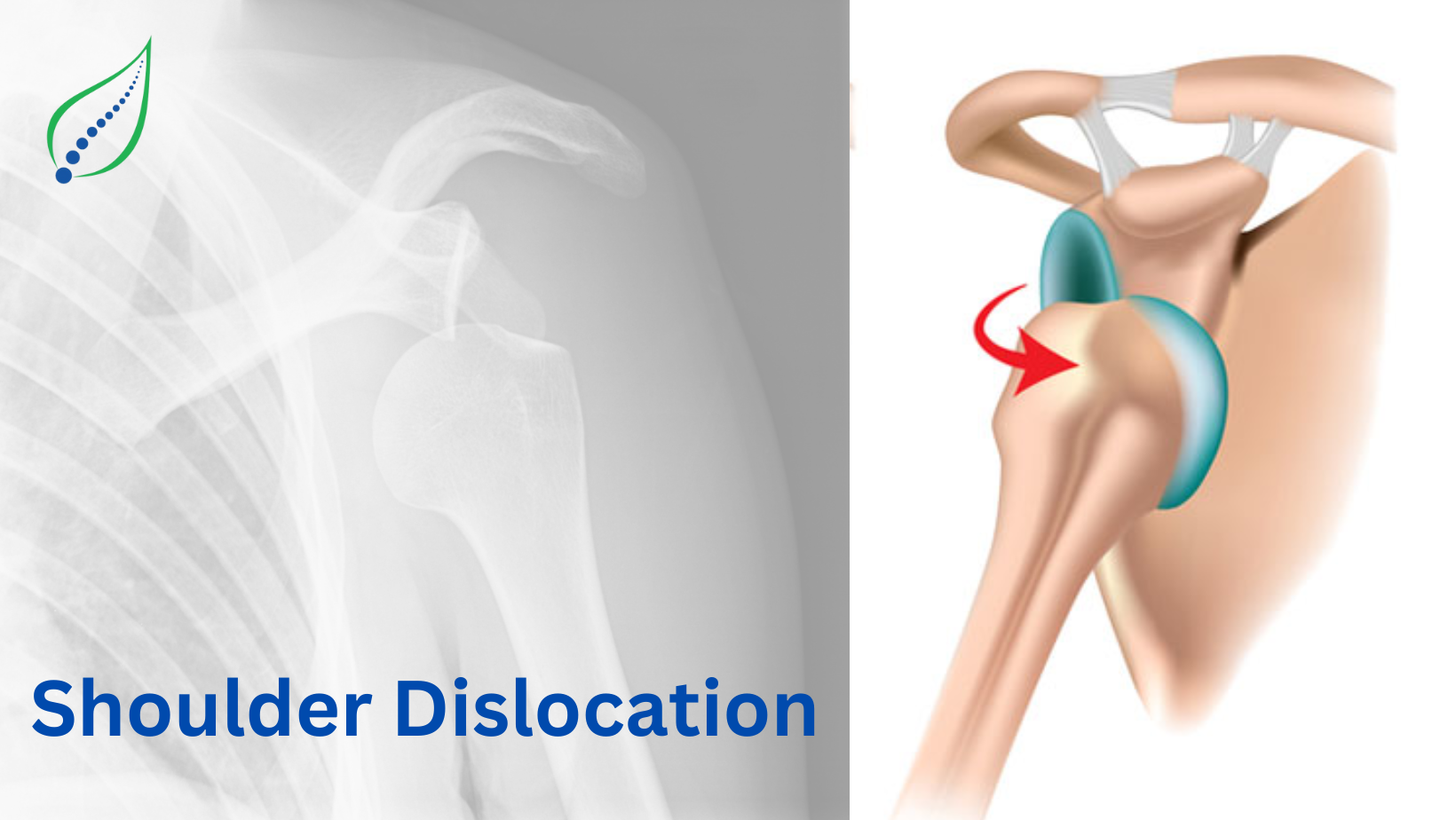
Shoulder Dislocation
Shoulder dislocation is one of the common orthopedic injuries where the head of the humerus is displaced from its normal position in the glenoid fossa of the scapula.
It is most commonly seen in clinical practice, especially in individuals who are active in sports activities such as football, hockey, or gymnastics, etc. Because of the wide range of motion and shallow socket, the shoulder joint is naturally prone to instability.
The shoulder joint is susceptible to instability due to a broad range of motion and a relatively shallow socket. Dislocations can cause significant pain, dysfunction, and long-term issues such as constant instability or chronic pain if poorly managed.
For an understanding of how the shoulder functions, it's important to start by looking at its anatomy.
The shoulder joint is also known as the glenohumeral joint. It is a type of synovial joint and ball and socket joint. This joint is made up of three types of bones: which scapula, the clavicle, and the humerus. The glenoid cavity is relatively shallow, which makes the shoulder highly dependent on surrounding soft tissues for stability.
The labrum, a fibro-cartilaginous rim, surrounds the glenoid cavity to help deepen it and stabilize the humeral head in order to compensate for the socket's shallowness.
The joint capsule and a group of ligaments, including the superior, middle, and inferior glenohumeral ligaments, as well as the coracohumeral ligament, provide more stability. The rotator cuff muscles, which include the supraspinatus, infraspinatus, teres minor, and subscapularis, play a crucial part in the shoulder's mobility and dynamic stability.
In addition, the bursae and synovial membrane inside the joint minimize friction while ensuring painless movement.
Because of its unique anatomical arrangement, the shoulder can perform a variety of motions, such as abduction, adduction, internal and external rotation, flexion, and extension. While the shoulder's extensive range of motion is a functional advantage, but due to this advantage it may compromise with the stability, and increasing the possibility of dislocations and other injuries.
Causes:
Basically, there are three different causes:
Traumatic (Commonest)
- Direct trauma, such as falls, collisions in high-impact sports, car accidents, or hard blows.
- Often seen in young, active individuals.
Atraumatic (non-traumatic):
1.Joint Hyper-mobility or joint laxity
2.Common in people with connective tissue disorders or repetitive overhead movements (e.g., swimmers, dancers).
3.These individuals may experience multi-directional instability and recurrent dislocations.
Pathological
1.Seizures or electrical injuries causing intense muscle contractions.
2.These are mostly caused by posterior dislocations.
Epidemiology:
- Shoulder dislocations are most frequent in males aged 18 to 30.
- Recurrent dislocations are extremely prevalent in younger people.
- Patients under 20 years mostly suffer from traumatic dislocation.
- Senior citizens > 60 may have dislocation as the outcome of minor trauma such as fall or getting hit by something.
- Participation in contact or overhead sports, contributes athletes to both initial and reoccurring shoulder dislocations.
It is very important to get a thorough clinical history and clinical examination for the identification and management of shoulder dislocation. It helps with the treatment and diagnosis.
The clinical examination plays a very important role as it helps in identifying the type of dislocation, assessing for associated injuries, and helps in further management. It involves inspection, palpation, assessing the range of motion, and neurovascular evaluation.
Clinical examination involves several steps, such as:
Inspection:
The injured shoulder often appears squared or flattened as a consequence of the deltoid failing to retain its position. This is caused by the humeral head shifting from the glenoid fossa.
The acromion is more prominent, and the humeral head may be palpated anteriorly in case of anterior dislocation or posteriorly in case of posterior dislocation.
The patient tries giving support to the affected arm with the opposite hand, avoiding movement due to pain.
Arm Position:
Depending upon the type of shoulder dislocation arm positing changes-
The most prevalent type is anterior dislocation, which appears with the arm held slightly abducted and externally rotated. In contrast, a posterior dislocation leads the patient to keep the arm adducted and internally rotated while actively preventing external rotation. In a rare the case of inferior dislocation, commonly referred to as luxatio erecta, the arm usually stays overhead in an abducted position.
Palpation
Palpation plays key clinical sign indicating that the joint is dislocated and helps it to differ from other shoulder injuries. As the humeral head is dislocated from the glenoid cavity, the glenoid fossa feels empty or hollow on palpation.
Range of Motion (ROM)
Restricted range of motion present on the affected side due to pain
Neurovascular assessments
Axillary Nerve is the most commonly injured during shoulder dislocation. Always make sure checking the sensation in the outer part of the shoulder and ask the patient to lift their arm sideways to check the deltoid muscle function.
Examine the radial, ulnar, and median nerves for tingling, numbness, or weakness in the forearm and hand, and ask the patient to actively move these areas. Also, palpate the radial pulse at the wrist to make sure that blood is flowing properly.
Also, a good quality XRAY is very important. But in some patient who play contact sports or who are recurrent dislocators for them MRI Or CT scan can also be advised to know if any soft tissues or any bony defects is involved respectively.
The three basic types of shoulder dislocation are characterized by the direction from which the humerus head slides out of the shoulder socket. These are:
Anterior dislocation:
It is the most common type representing more than 90% of instances. In this condition the humeral head moves forward, typically under the coracoid process.
The main cause is any kind of traumatic injury, such as a fall on an outstretched hand or while engaging in any contact sports.
In this condition, the arm is held slightly apart from the body, with external rotation.
Some complications:
a. Bankart Lesion (Labral Tear)
b. Hill-Sachs lesion (compression fracture of the humerus head)
Posterior dislocation:
It is the least common almost about 2-4% of cases are noticed.
In this condition the humeral head moves behind the glenoid cavity.
And it is often triggered by seizures, electric shock, or a direct impact to the front of the shoulder.
In posterior dislocation, the arm is held in internal rotation; exterior rotation is substantially restricted.
The main challenge in this condition is missed diagnosis as it is frequently missed on ordinary X-rays therefore special views may be required.
Inferior Dislocation (Luxatio Erecta)
It is the rarest kind of dislocations (less than 1% of shoulder dislocations).
In this condition the humeral head is shifted downwards and below the glenoid. It is caused by sudden strong hyperabduction for example when an arm is pulled overhead with force).
In conditions such as inferior dislocation, the arm is raised overhead with elbow flexed and forearm pronated.
Its common complications include nerve or vascular injury caused by traction forces.
Some of the non-surgical treatments can be done such as:
- Closed Reduction
A healthcare professional gently manipulates the arm to reattach the dislocated humeral head into its socket. It is usually done under sedation or local anesthetic. - Immobilization
Post reduction, the shoulder is held still with a sling or brace for 1-3 weeks (length varies depending upon severity and age). It helps to rest the joint and minimize inflammation. - Pain Management
Pain and swelling is initially managed by using NSAIDs. - Physical Therapy and Rehabilitation
It starts after the initial immobilization phase.
The main focus is restoring range of motion, strengthening the rotator cuff and shoulder stabilizers.
The most important task is to improve joint proprioception (body awareness). - Activity Modification
Avoid any kind of high-risk movements or activities that might result in another dislocation, particularly during the recovery phase.
What are the preventive measures in Shoulder Dislocation:
- Strengthening Exercises
It plays an important part in healing and maintaining. Therefore, regular shoulder and upper back strengthening should be done, specifically in the rotator cuff and scapular muscles, this improves joint stability. - Proper Warm-up and Stretching
Always make sure of doing warm up before any kind of strenuous activity or sports as muscle and ligament training is essential. - Avoid risky movements.
Being cautious when performing any activity or powerful arm movements, particularly when there is a history of dislocation. - Posture Correction
Maintaining good shoulder position throughout daily tasks and exercises reduces stress on the joint. - Protective Gear
Always wear shoulder braces or supports during contact sports to increase stability. - Regular Follow-up
If you've had a previous dislocation, continuous monitoring and therapy might help identify early indicators of instability.